Humanized mouse models have emerged as indispensable tools in immuno-oncology research, providing valuable insights into the complexities of the human immune system and its interaction with cancer. These models involve engrafting human immune cells or tissues into immunocompromised mice, creating a platform to study human immune responses in a living organism. This article delves into the significance of humanized mouse models for advancing our understanding of cancer immunology and facilitating the development of novel immunotherapies.
The Advantages of Humanized Mouse Models
Traditional preclinical cancer models, often relying on cell lines or syngeneic mouse models, lack the complexity of the human immune system. Humanized mouse models bridge this gap by providing a more physiologically relevant environment to:
- Investigate Human Immune Responses: These models allow researchers to study the interactions between human immune cells, such as T cells and NK cells, and tumor cells in a living system.
- Evaluate Immunotherapy Approaches: Humanized mouse models serve as a platform to test the efficacy and safety of novel immunotherapies, including CAR T-cell therapy and immune checkpoint inhibitors.
- Study Tumor Microenvironment: The interaction between tumor cells and the surrounding microenvironment is crucial for tumor growth and metastasis. Humanized models help dissect the role of human immune cells within the tumor microenvironment.
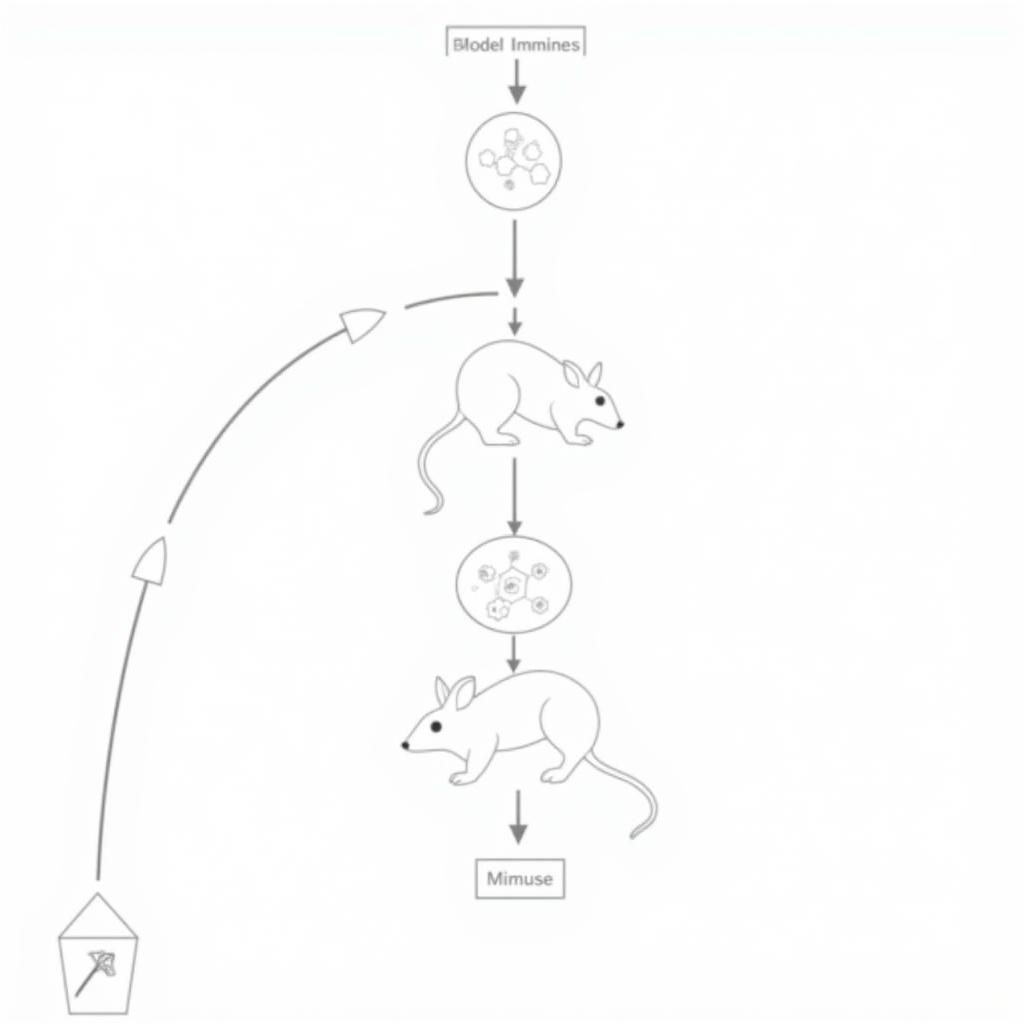 Humanized Mouse Model Illustration
Humanized Mouse Model Illustration
Types of Humanized Mouse Models
Various humanized mouse models are utilized in immuno-oncology research, each with its advantages and limitations. Some common types include:
- Hu-PBL Mice: These models involve injecting human peripheral blood lymphocytes (PBLs) into immunodeficient mice.
- Hu-SRC Mice: Human stem cell reconstitution (SRC) models involve engrafting human hematopoietic stem cells, which differentiate into various human immune cells.
- Bone Marrow-Liver-Thymus (BLT) Mice: BLT mice receive human fetal liver and thymus tissue implants along with hematopoietic stem cells, leading to a more complete human immune system.
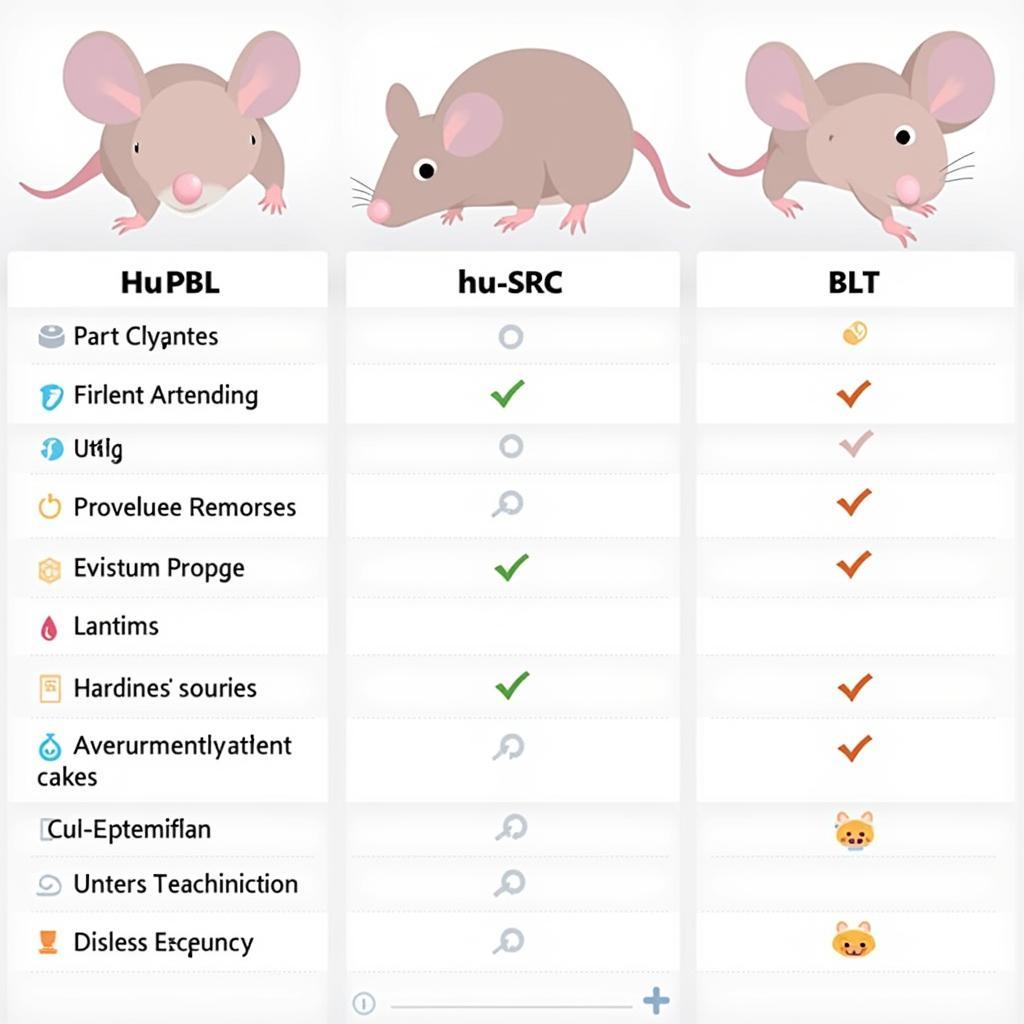 Comparison of Humanized Mouse Models
Comparison of Humanized Mouse Models
Applications in Immuno-Oncology Research
Humanized mouse models have become indispensable in various areas of immuno-oncology research:
- Drug Discovery and Development: These models play a crucial role in preclinical drug testing, enabling researchers to evaluate the efficacy, safety, and pharmacokinetics of novel immunotherapies in a humanized setting.
- Personalized Medicine: Humanized mouse models are being explored for personalized medicine approaches, where a patient’s tumor cells and immune cells are used to create a model that mimics their unique disease.
- Understanding Mechanisms of Immune Evasion: These models help researchers study how tumor cells evade the immune system and develop strategies to overcome these mechanisms.
“Humanized mouse models have revolutionized the field of immuno-oncology,” says Dr. Emily Carter, a leading researcher in cancer immunology. “These models provide an unparalleled tool to study the complexities of the human immune system in the context of cancer and are instrumental in developing new and effective immunotherapies.”
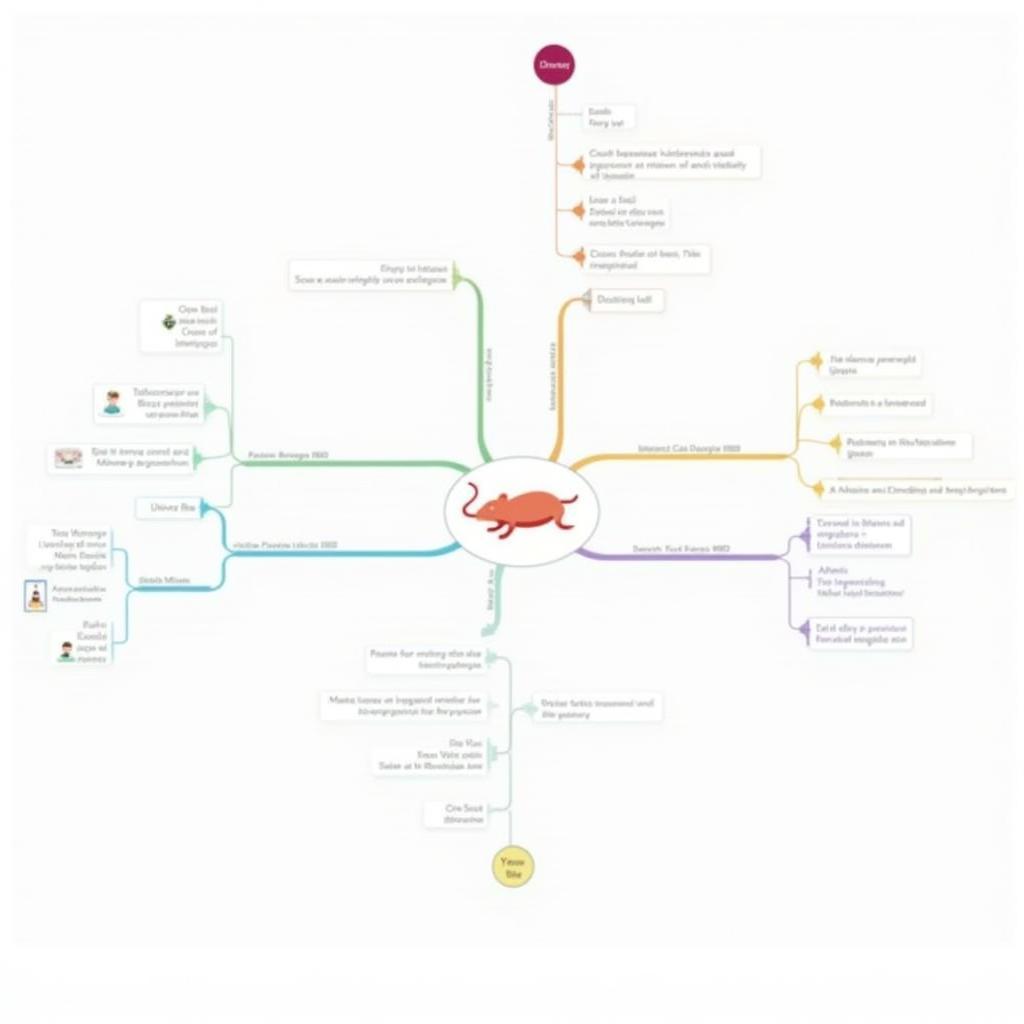 Applications of Humanized Mouse Models
Applications of Humanized Mouse Models
Conclusion
Humanized mouse models have become essential tools for advancing our understanding of cancer immunology and developing effective immunotherapies. As these models continue to evolve and improve, they hold immense promise for developing personalized cancer treatments and improving patient outcomes.